Care for Patient With Hematologic Problem Hesi Review
Care of Patients with Hematologic Disorders
Objectives
Theory
Clinical Practice
Central Terms
allogeneic (ĂL-ō-JĔN-ĭk, p. 364)
anemia (ă-NĒ-mē-ă, p. 346)
autologous (ăw-TŎL-ŏ-gŭs, pp. 362, 364)
disseminated intravascular coagulation (DIC) (dĭ-SĔM-ĭ-nāt-ĕd ĭn-tră-VĂS-cū-lăr kō-ăg-ū-LĀ-shŭn, p. 362)
ecchymoses (ĕk-ĭ-MŌ-sēz, p. 359)
hemarthrosis (hē-măr-THRŌ-sĭs, p. 361)
hemolysis (hē-MŎL-ĭ-sĭs, p. 347)
hypovolemia (hī-pō-vō-LĒ-mē-ă, p. 346)
leukapheresis (lū-kă-fĕ-RĒ-sĭs, p. 356)
purpura (PŬR-pū-ră, p. 359)
splenomegaly (splē-nō-MĒG-ă-lē, p. 354)
stomatitis (stō-mă-TĪ-tĭs, p. 359)
thrombocytopenia (thrŏm-bō-sīt-ō-PĒ-nē-ă, p. 359)
 evolve.elsevier.com/deWit/medsurg
evolve.elsevier.com/deWit/medsurg
Disorders of the Hematologic System
Anemia
In the human being body, healthy reddish blood cells (RBCs) deport oxygen to tissues. A residuum is maintained between the production of new RBCs and the disposal of old "worn-out" RBCs. Anemia occurs when something interferes with this balance or interferes with the maturation of cells. Anemia is a state in which there are insufficient numbers of functioning RBCs, or a lack of hemoglobin, to encounter the demands of the tissues for oxygen.
Etiology
There are 3 major classifications of anemia, according to cause:
Rapid, astringent bleeding leads to anemia from blood loss, hypovolemia (decreased volume of circulating claret), and, potentially, daze. A blood loss that leads to anemia may result from astringent trauma to the blood vessels and massive hemorrhage or the blood loss may be more gradual, every bit from a pocket-size, haemorrhage peptic ulcer that causes a chronic blood loss.
The amount of blood loss that leads to hypovolemic shock varies, depending on the ability of the patient's body to recoup for the lost fluid volume. A blood loss of even 500 mL in an developed who had normal circulating volume may cause hypovolemic stupor. See Chapter 45 for the treatment of shock. Tabular array 17-1 shows the amount of blood loss and consequent clinical manifestations.
Tabular array 17-1
Clinical Manifestations of Acute Blood Loss
| Volume Lost | Clinical Manifestations |
| ten% | None |
| twenty% | At rest, no signs or symptoms; slight postural hypotension when standing; tachycardia with exercise |
| thirty% | Claret pressure and pulse normal when supine; postural hypotension and tachycardia with exercise |
| xl% | Below-normal blood force per unit area, key venous pressure, and cardiac output at remainder; rapid, thready pulse and common cold, damp pare |
| 50% | Shock and potential death |
Adapted from Lewis, S.Fifty., Heitkemper, M.M., Dirksen, S.R., et al. (2007). Medical-Surgical Nursing: Assessment and Management of Clinical Problems (7th ed.). St. Louis: Mosby, p. 695.
Anemia caused by a failure in cell production is the outcome of either a deficiency of certain substances necessary for the formation of RBCs, or results from the abnormal office of bone marrow. Examples of this type of anemia are:
Iron or folic acid may not be well absorbed in people who have an intestinal malabsorption syndrome.
Hemolytic anemias, in which blood-red cells are destroyed prematurely in the body, take many causes. Hemolytic anemia tin be a result of genetic defects that affect jail cell construction, causing the cells to atomize quickly. Some of the hemolytic anemias, such as thalassemia, are inherited, whereas others are caused when erythrocytes are exposed to poisonous agents, such as chemicals or certain bacterial toxins.
Allowed reactions can crusade blood cell hemolysis (destruction of red cells). The presence of toxins in the blood, infections such as malaria, transfusion reactions, and changes in blood chemistry may cause blood-red cell hemolysis. Blood incompatibility in the newborn (erythroblastosis fetalis) is another cause.
Pathophysiology
Iron deficiency anemia occurs when full torso iron is insufficient and erythropoiesis is macerated. The lack of iron impedes the formation of hemoglobin (Hb) (Concept Map 17-1). In pernicious anemia, an autoimmune disease, the intrinsic factor is missing from the gastric juices, and vitamin B12 is not absorbed without it. Vitamin B12 acts as a coenzyme in conjunction with folate metabolism and is important in the utilization of iron and poly peptide for the manufacture of RBCs. The result of the missing intrinsic factor is that the red cell production is decreased, and those red cells that are produced are aberrant in their structure and role (Concept Map 17-2). To correct this condition, the physician will gild the assistants of vitamin B12. A folic acrid deficiency also contributes to anemia (Gentili et al., 2009).
Hemolytic anemias associated with excessive destruction of RBCs are quite rare. When red cells are not normal, they suspension up easily or are destroyed by the trunk more than quickly than are normal red cells. This RBC devastation causes the anemia.
Anemia occurs in end-stage renal disease patients when there is a deficiency of production of erythropoietin, a substance necessary to stimulate the production of RBCs in the bone marrow. This problem is unremarkably corrected by the assistants of epoetin alfa (Epogen), which stimulates crimson cell production (Singh, 2006). Oxygen ship depends on the number and condition of the red cells and the amount of hemoglobin they contain.
Signs and Symptoms
Signs and symptoms of anemias from causes other than rapid bleeding depend on whether the anemia is balmy, moderate, or severe. Signs and symptoms of mild anemia (Hb nine.five to xiii 1000/dL) are mild headache, palpitations, and dyspnea on exertion. Moderate anemia (Hb six to 10 g/dL) may include brittle nails, sore natural language, pallor, chronic fatigue, headache, and dizziness or faintness. Tabular array 17-two presents the many signs and symptoms of severe anemia. Tachypnea and tachycardia may develop with severe anemia due to the decreased power of the blood to transport sufficient oxygen to the tissues.
Tabular array 17-two
Signs and Symptoms of Severe Anemia
| Body System | Signs and Symptoms |
| General | Sensitivity to cold, lethargy, weight loss |
| Eyes | Blurred vision, blue colored sclera, yellowing of conjunctiva or pale conjunctiva, retinal hemorrhage |
| Skin | Pallor of face up and palms, pruritus, jaundice, pale nail beds, pale mucous membranes, stomatitis, breakable nails, cheilitis |
| Cardiovascular | Palpitations, tachycardia, angina, systolic murmur, widened pulse force per unit area, intermittent claudication, CHF, possible MI |
| Respiratory | Tachypnea, orthopnea, dyspnea at rest |
| Gastrointestinal | Anorexia, difficulty swallowing, glossitis, enlarged liver, enlarged spleen, smooth natural language |
| Musculoskeletal | Os pain |
| Neurologic | Headache, dizziness, impaired thinking, irritability, low, fatigue |
CHF, congestive heart failure; MI, myocardial infarction.
Diagnosis
The microscopic appearance of the red cells in a motion-picture show of blood that has been spread over a slide (a peripheral smear) gives information about abnormalities in size, shape, and color of erythrocytes circulating in the patient's bloodstream. The complete blood count (CBC) and differential prison cell count results are used to diagnose the presence of anemia. Measuring the quantity of hemoglobin tells whether the cells take sufficient amounts of hemoglobin to comport adequate oxygen to the trunk.
The prefix normo- refers to normal; the suffix -cyte refers to cells; the suffix -chrom refers to color; and the suffix –ic ways "having the quality of" or "characterized past." Thus a normocytic, normochromic anemia is characterized past cells that are normal in size and color, but that take a deficiency in the number of RBCs and a low hematocrit. This type of anemia ordinarily occurs every bit a result of sudden blood loss.
A hypochromic, microcytic anemia is characterized by decreased levels of hemoglobin (not enough color) and small-scale (micro) cells. This type of anemia is typical of an iron deficiency anemia.
Handling
Anemia from chronic, slow claret loss is treated by correcting the underlying problem and and then building replacement blood cells. Anemia acquired past inadequate iron, folic acid, or poly peptide intake is managed with oral iron supplements, vitamins, and nutrition aligning. If the anemia is serious, blood transfusions may be given, or fe supplementation may be administered intravenously (IV) with iron dextran (Imferon), sodium ferrous gluconate, or iron sucrose.
Pernicious anemia is treated by regular injections of vitamin B12, or by weekly use of an intranasal form of cyanocobalamin (Nascobal), every bit the deficiency of intrinsic cistron prevents acceptable absorption of this vitamin from food. At that place should be sufficient folic acid in the nutrition or by supplement. Tabular array 17-3 presents the medications most commonly prescribed for hematologic disorders.
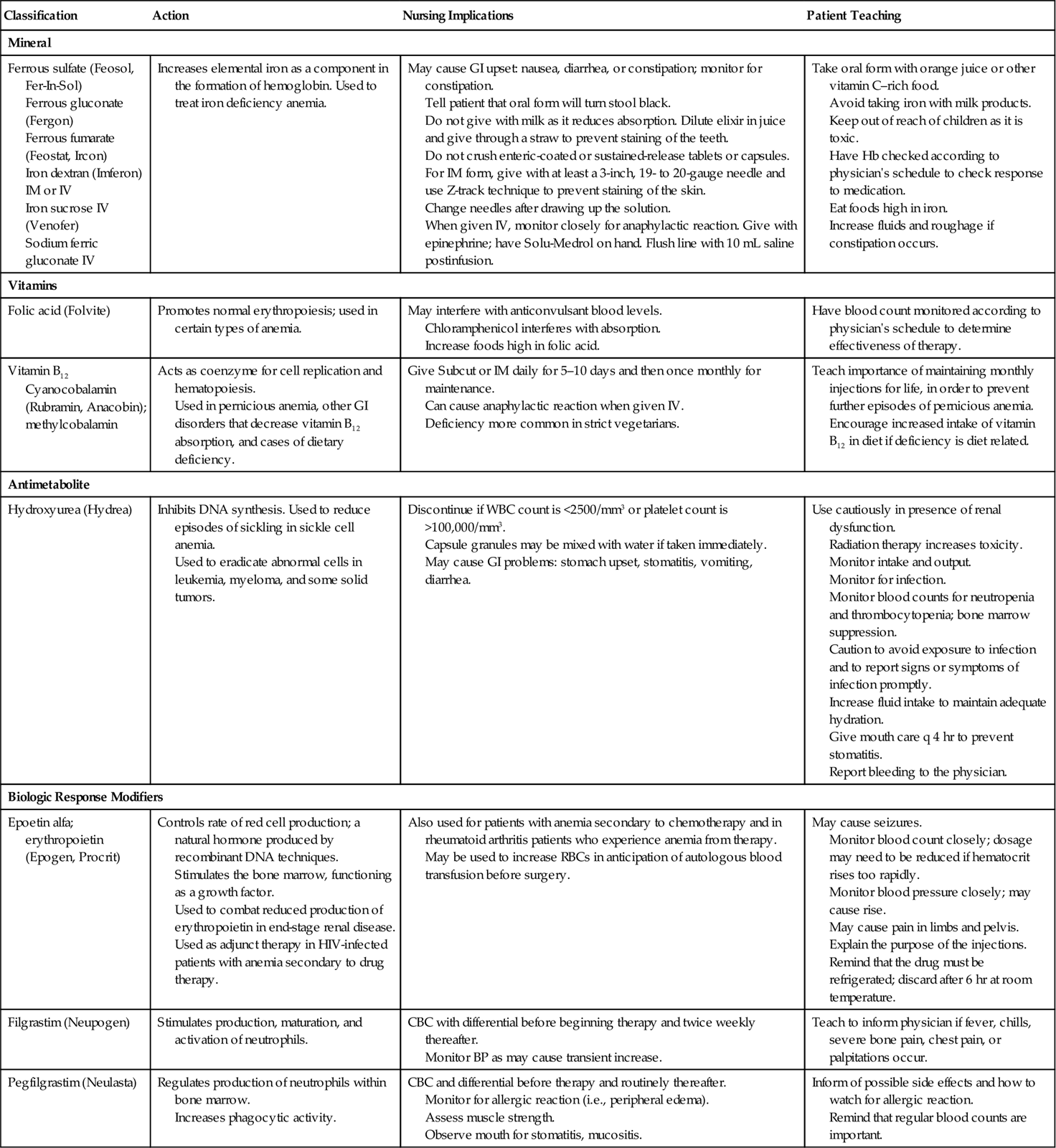
Medications Commonly Prescribed for Disorders of the Hematologic Arrangement* BP, blood pressure level; CBC, complete blood count; GI, gastrointestinal; Hb, hemoglobin; HIV, human immunodeficiency virus; IM, intramuscularly; 4, intravenously; RBCs, red claret cells; Subcut, subcutaneously; WBC, white blood cell. * Chemotherapy drugs are presented in Chapter viii. Table 17-iii
Table 17-iii
Classification Action Nursing Implications Patient Teaching Mineral Ferrous sulfate (Feosol, Fer-In-Sol)
Ferrous gluconate (Fergon)
Ferrous fumarate (Feostat, Ircon)
Iron dextran (Imferon) IM or 4
Fe sucrose IV (Venofer)
Sodium ferric gluconate 4Increases elemental iron every bit a component in the formation of hemoglobin. Used to treat iron deficiency anemia. May cause GI upset: nausea, diarrhea, or constipation; monitor for constipation.
Tell patient that oral form will turn stool blackness.
Do not requite with milk every bit information technology reduces absorption. Dilute elixir in juice and give through a straw to prevent staining of the teeth.
Do non crush enteric-coated or sustained-release tablets or capsules. For IM form, give with at least a 3-inch, xix- to xx-gauge needle and use Z-track technique to prevent staining of the pare.
Change needles after drawing upwards the solution.
When given 4, monitor closely for anaphylactic reaction. Give with epinephrine; take Solu-Medrol on manus. Affluent line with 10 mL saline postinfusion.Have oral class with orange juice or other vitamin C–rich food.
Avert taking iron with milk products.
Keep out of reach of children as it is toxic.
Have Hb checked according to physician's schedule to cheque response to medication.
Consume foods high in iron.
Increase fluids and roughage if constipation occurs. Vitamins Folic acid (Folvite) Promotes normal erythropoiesis; used in certain types of anemia. May interfere with anticonvulsant blood levels.
Chloramphenicol interferes with absorption.
Increase foods high in folic acid.Take blood count monitored co-ordinate to physician's schedule to make up one's mind effectiveness of therapy. Vitamin B12 Cyanocobalamin (Rubramin, Anacobin); methylcobalamin Acts equally coenzyme for cell replication and hematopoiesis.
Used in pernicious anemia, other GI disorders that subtract vitamin B12 absorption, and cases of dietary deficiency.Give Subcut or IM daily for 5–10 days and and then one time monthly for maintenance.
Tin cause anaphylactic reaction when given IV.
Deficiency more common in strict vegetarians.Teach importance of maintaining monthly injections for life, in society to prevent farther episodes of pernicious anemia.
Encourage increased intake of vitamin B12 in diet if deficiency is nutrition related. Antimetabolite Hydroxyurea (Hydrea) Inhibits Deoxyribonucleic acid synthesis. Used to reduce episodes of sickling in sickle cell anemia.
Used to eradicate abnormal cells in leukemia, myeloma, and some solid tumors.Discontinue if WBC count is <2500/mmiii or platelet count is >100,000/mmiii.
Capsule granules may be mixed with water if taken immediately.
May cause GI problems: stomach upset, stomatitis, vomiting, diarrhea.Use cautiously in presence of renal dysfunction.
Radiation therapy increases toxicity.
Monitor intake and output.
Monitor for infection.
Monitor blood counts for neutropenia and thrombocytopenia; os marrow suppression.
Circumspection to avoid exposure to infection and to study signs or symptoms of infection promptly.
Increase fluid intake to maintain adequate hydration.
Requite oral fissure intendance q 4 hr to prevent stomatitis.
Report bleeding to the physician. Biologic Response Modifiers Epoetin alfa; erythropoietin (Epogen, Procrit) Controls rate of red prison cell production; a natural hormone produced by recombinant DNA techniques.
Stimulates the os marrow, operation as a growth gene.
Used to gainsay reduced production of erythropoietin in end-stage renal affliction.
Used as adjunct therapy in HIV-infected patients with anemia secondary to drug therapy.Also used for patients with anemia secondary to chemotherapy and in rheumatoid arthritis patients who experience anemia from therapy.
May be used to increment RBCs in anticipation of autologous blood transfusion before surgery.May cause seizures.
Monitor claret count closely; dosage may demand to be reduced if hematocrit rises also rapidly.
Monitor blood force per unit area closely; may cause rise.
May crusade pain in limbs and pelvis.
Explain the purpose of the injections.
Remind that the drug must be refrigerated; discard subsequently six hr at room temperature. Filgrastim (Neupogen) Stimulates production, maturation, and activation of neutrophils. CBC with differential before beginning therapy and twice weekly thereafter.
Monitor BP equally may cause transient increase.Teach to inform physician if fever, chills, severe bone hurting, chest pain, or palpitations occur. Pegfilgrastim (Neulasta) Regulates product of neutrophils within os marrow.
Increases phagocytic activity.CBC and differential before therapy and routinely thereafter.
Monitor for allergic reaction (i.e., peripheral edema).
Assess musculus strength.
Discover mouth for stomatitis, mucositis.Inform of possible side effects and how to lookout for allergic reaction.
Remind that regular blood counts are important.
For hemolytic anemia, the underlying cause is found and corrected (if possible) and then the blood volume is rebuilt with added iron and appropriate nutrition. If the anemia is severe, claret transfusion may be indicated.
Nursing Management
Assessment (Data Collection)
Whenever a patient complains of fatigue, headaches, or shortness of jiff, anemia should always exist considered. Besides the CBC results, data regarding physical signs and symptoms are collected.
Nursing Diagnosis
Nursing diagnoses are chosen based on the clinical findings and issues identified. Mutual nursing diagnoses include:
Planning
Expected outcomes are written for the specific individual nursing diagnoses chosen to resolve the patient'south problems. For the nursing diagnoses listed above, outcomes might include:
Implementation
Intervention is based on an understanding of the detail kind of anemia affecting the patient. Anemia from blood loss presents bug quite unlike from those related to chronic—and possibly incurable—aplastic or hemolytic anemia. For patients with anemias that interfere with clotting and that tend to cause bleeding episodes, nursing actions are directed toward preventing the episodes. For any patient with anemia severe plenty to crusade fatigue, assist with daily living activities, and provide planned rest periods.
Nursing functions include administering claret, iron, vitamin B12, and folic acid and monitoring for desired effects. Patients are educated about needed dietary adjustments. Patients should be taught that iron is captivated more readily if vitamin C is simultaneously nowadays in the gastrointestinal (GI) system. Taking fe medication with orange juice provides the necessary vitamin C.
Analgesia for headache or articulation hurting is given as ordered, and the patient is monitored for adverse side effects. More than nursing diagnoses commonly associated with hematologic problems, including anemia, and lists of advisable interventions are included in Table 16-two.
Evaluation
Evaluation data are gathered to determine whether expected outcomes are existence met. Laboratory values are particularly important when evaluating the intendance of the patient with anemia. However, equally important are data showing that the bug caused by the anemia are resolving.
Aplastic Anemia
Aplastic anemia (a rare disorder) may develop after a viral infection, as a reaction to a drug, or because of an inherited trend. The illness is characterized by os marrow depression and is idea to probably exist an immune-mediated illness. Ruby cells, white cells, and platelet levels are decreased. The toxic effects of sure substances can be responsible for aplastic anemia. Some of these agents include benzene; insecticides; drugs, such as chloramphenicol (Chloromycetin), phenylbutazone (Butazolidin), and sulfonamides; some anticonvulsants; gold compounds used to care for rheumatoid arthritis; and alkylating agents or antimetabolites used in chemotherapy. Many other drugs  can cause aplastic anemia, but this agin result is rare. Radiation exposure is another factor in the development of the disorder.
can cause aplastic anemia, but this agin result is rare. Radiation exposure is another factor in the development of the disorder.
Impairment or failure of os marrow function leading to the loss of stem cells is the cause of aplastic anemia (Concept Map 17-3). With aplastic anemia, the bone marrow has decreased cells and increased fatty tissue. In addition to the signs and symptoms of iron deficiency anemia, ecchymosis, petechiae, and hemorrhage related to low platelet count also occur. Infection is frequent and may not cause an inflammatory response because of the very low leukocyte count. At that place is often frequent bleeding in the mouth.
Diagnosis is by claret count with differential, os marrow biopsy, and ruling out other disorders. Aplastic anemia causes an emergency state of affairs. Handling must eliminate any identifiable underlying cause. Packed crimson cells and platelets are administered. Antibiotics are given for identified infection; oxygen is sometimes administered to patients with low erythrocyte counts. Os marrow transplantation (BMT) is the handling of choice for those under 45 years of age with severe bone marrow depression, but there must exist an identical human leukocyte antigen (HLA) match. Immunosuppressive therapy with antithymocyte globulin (ATG) and cyclosporine is showing hope at improving outcomes. ATG contains polyclonal antibodies against human T cells.
Prevention of hemorrhage and infection is a top priority. Psychological support of the patient and family is of import when they are faced with this life-threatening status. Safe measures are priorities. Actions for problems of weakness and fatigue are the same equally those presented for anemia earlier in the chapter. Other common nursing interventions are included in Tabular array xvi-2. See Chapter 8 and the Evolve website for precautions and deportment for the patient with leukopenia and neutropenia and for prophylactic measures when thrombocytopenia is  present.
present.
Sickle Jail cell Affliction
Etiology
Sickle cell disease is a genetic disorder in which the gene is inherited from both parents (homozygous gene) (Table 17-4). Sickle cell disease is characterized by erythrocytes that contain more hemoglobin S than hemoglobin A. Sickle cell disease is establish in less than 1% of African American newborns, merely also affects some people whose ancestors are from the Mediterranean region, the Middle Eastward, and Bharat. Approximately viii% of African Americans carry the gene.
from both parents (homozygous gene) (Table 17-4). Sickle cell disease is characterized by erythrocytes that contain more hemoglobin S than hemoglobin A. Sickle cell disease is establish in less than 1% of African American newborns, merely also affects some people whose ancestors are from the Mediterranean region, the Middle Eastward, and Bharat. Approximately viii% of African Americans carry the gene.
Sickle prison cell trait, in which simply near l% of an private's total hemoglobin is affected, is present in well-nigh 10% of the African American population of the United states of america. The trait is heterozygous, significant that the person has an inherited gene for the trait from one parent only. People with the heterozygous trait for sickle cell are carriers; they can transmit the factor to their children even when they themselves practise not testify signs of the disease. Therefore, genetic counseling and acceptable screening for early detection of the disease are considered extremely important to control sickle cell anemia. In the United states of america, many patients with sickle jail cell anemia live into their mid-40s. The most common cause of expiry is astute breast syndrome, where damage occurs to the lungs.
Pathophysiology
When the patient with sickle cell disease experiences lower oxygenation than normal, the defective South hemoglobin forms clumps in the ruby cells, causing them to assume a sickle shape, blocking blood vessels, breaking apart, and forming thrombi that cause organ harm. Sickle cells are destroyed past the body very quickly, causing anemia.
Sickle cell trait occurs in people who take only one cistron, rather than a pair of genes, for sickle cell anemia. They unremarkably exercise non have problems with cells assuming a sickle shape unless they feel severe oxygen deficiency.
Signs and Symptoms
The signs and symptoms of sickle cell disease are those that indicate lack of oxygen and blood catamenia, such equally pallor, lethargy, and pain. The problems from interrupted normal blood flow bear upon many organs (Figure 17-2). Painful swelling of the hands and feet related to bone infarction from the sickled cells (manus-foot syndrome) may occur. Afterward sickle cell crunch, signs typical of anemia occur considering the abnormally shaped cells are very fragile, break easily, and are destroyed. The RBC and hemoglobin counts tin drib very speedily during a crunch.
Diagnosis
A peripheral claret smear tin can show sickled cells. The sickling examination, which exposes RBCs to a deoxygenating amanuensis, is diagnostic. Hemoglobin electrophoresis identifies the presence of abnormal hemoglobin. During crisis, there volition be elevations of serum bilirubin because of the hemolysis of the abnormal red cells. Bone and articulation abnormalities are revealed by skeletal ten-rays.
Handling
At that place is no cure or specific handling for sickle cell anemia; handling is primarily symptomatic and preventive. Patients should be taking folic acid regularly and eating a diet with sufficient poly peptide to help build cerise cells. Infection is to be avoided, and the patient should receive all recommended immunizations against influenza, hepatitis A and B, pneumonia, tetanus, and the like. Adequate intake of fluid on a daily basis is important to keep the claret every bit fluid as possible. Booze and recreational drugs are to be avoided every bit they can cause complications. Quick attention for illness should exist sought.
The drug hydroxyurea (Hydrea) has been institute to reduce the frequency of sickling episodes. Patients on this drug take shown a l% decrease in the number of hospitalizations for crunch (Platt, 2008). Sodium cromoglycate given by inhalation or via nasal road has been shown to significantly reduce the percentage of cells that sickle in venous blood (Bizumukama et al., 2009). If a crisis occurs, the patient may be treated at home with bed rest, acceptable fluid intake, and analgesics. Pain control is of import during a crunch. Narcotic analgesia with morphine is administered on a continuous basis, unremarkably by patient-controlled analgesia pump. If the patient's hemoglobin drops considerably or his condition all of a sudden deteriorates, he is hospitalized, given oxygen, and transfused with packed red cells; in improver, IV fluids are given. An attempt is fabricated to mobilize the sickled cells and to prevent damage to major organs. Infection is treated with appropriate antibiotics.
There are many complications of sickle cell disease, including cholecystitis, stroke, congestive heart failure, and harm to all major organs (Figure 17-3). One of the nigh common problems is leg ulcers, from impaired circulation to the legs and feet. Protecting the feet and lower legs from injury is important, since small wounds tend to develop into difficult-to-heal ulcers.
BMT is the only available treatment that can cure some patients. The scarcity of donors, the cost, and the risks involved greatly limit the use of this choice. Gene therapy is offering hope for future treatment of sickle cell disease.
Nursing Management
Nursing care is aimed at relieving the symptoms from complications of the illness and minimizing organ damage. Patients are taught to avert high altitudes, vigorous exercise, and iced liquids. Patients are to maintain acceptable fluid intake, refrain from smoking, and obtain treatment for infections promptly. Acceptable rest is important as patients with sickle cell anemia experience fatigue. Assessment for acceptable hurting relief is a elevation priority  (Arnold & Besa, 2010). Intake and output will be monitored to prevent overloading the patient with fluid. Oxygen therapy is instituted if the patient is hypoxic (oxygen therapy helps foreclose farther cellular
(Arnold & Besa, 2010). Intake and output will be monitored to prevent overloading the patient with fluid. Oxygen therapy is instituted if the patient is hypoxic (oxygen therapy helps foreclose farther cellular damage).
damage).
Polycythemia Vera
Excessive production of RBCs results in polycythemia vera. White cell numbers also increase, merely not to the degree that they do in leukemia. The cause of polycythemia vera is unknown, simply the disease is considered a neoplastic disorder. The blood becomes thick from the increased numbers of cells, blood vessels become distended, and blood flow is sluggish. Because of the sluggish menses, there is a trend to develop blood clots. Blood pressure is elevated and the heart hypertrophies. Hemorrhage is frequent in areas of distended blood vessels. Signs and symptoms of polycythemia vera include a reddish face with deep-red purplish lips, fatigue, weakness, dizziness, headache, enlarged spleen (splenomegaly), and congested liver. Minor injury may result in excessive bleeding.
Handling is aimed at reducing the number of blood cells. Phlebotomy, antineoplastic agents, and radiation therapy are all used. In phlebotomy, a claret vessel is pierced, and blood is fatigued off. Equally much equally 500 mL of blood at a fourth dimension may be withdrawn every two to three months. Increased fluid intake is essential to decrease blood viscosity, and aspirin is used to decrease platelet clumping and clot formation.
A secondary polycythemia may develop in response to prolonged hypoxia and increased erythropoietin secretion. Secondary polycythemia does not have the same effects as principal polycythemia.
Leukemia
The word leukemia, translated literally, ways "white blood." Actually, the white blood cells (WBCs) would accept to number ane,000,000/mm3 before the claret would have a milky white appearance, and, although leukemia is characterized by an increase in the number of leukocytes, their number rarely rises above 500,000/mm3. In addition to the increment in number, however, the leukocytes of the patient with leukemia are abnormal cells that do not office as normal white cells do.
Etiology
Leukemia is a cancer, and as with other types of cancers, the verbal cause of leukemia is non known. There are factors considered to be closely linked with the development of leukemia. Exposure to ionizing radiation in relatively large doses is one such gene. Another is exposure to certain chemicals, such every bit benzene, that are toxic to os marrow. Benzene is an ingredient in atomic number 82-free gasoline, and the incidence of leukemia has risen since lead-free gasoline has been in use. The amount of exposure to benzene and other chemicals that causes bone marrow suppression is unknown, and this corporeality possibly varies among individuals. The point is to be careful about animate gasoline fumes and using household chemicals and pesticides. The third factor is the retrovirus known as man T-lymphotropic virus 1 (HTLV-1), which causes homo T-cell leukemia. People with an abnormal number of chromosomes and chromosomal translocations are at a greater run a risk for developing acute lymphocytic leukemia. Almost ninety% of patients with chronic myelogenous leukemia have the Philadelphia chromosome.
Malignant production of WBCs is the actual cause of the disease. Dna become damaged. Tabular array 17-5 shows the clinical manifestations of leukemia and the factors linked to their development.
Table 17-v
Causes of Clinical Signs of Leukemia
| Manifestations | Causes |
| Astringent infections | Immature and abnormally functioning leukocytes, even though at that place is an increased number of them. |
| Symptoms of anemia | Rapidly proliferating white cells apparently "crowd out" developing red cells and platelets. |
| Enlarged spleen, liver, and lymph nodes | Excess white cells accumulate within organs, causing distention of tissues. |
| Weakness, pallor, and weight loss due to elevated metabolic rate | Increased production of white cells requires large amounts of amino acids and vitamins. Increased destruction of cells leads to more metabolic wastes that must exist tending of by the trunk. |
| Renal pain, urinary stones and obstruction to flow of urine, and urinary tract infection | Large amounts of uric acid are released when white cells are destroyed past antileukemic drugs. |
| Headache, disorientation, and other fundamental nervous system symptoms | Abnormal white cells infiltrate the central nervous organization. |
Source: https://nursekey.com/17-care-of-patients-with-hematologic-disorders/

0 Response to "Care for Patient With Hematologic Problem Hesi Review"
Post a Comment